REPORTS
Melanoma Update 2018
Presented by: Allan C. Halpern, MD, FAADChief, Dermatology Service, Memorial Sloan Kettering Cancer Center, New York, NY, USA
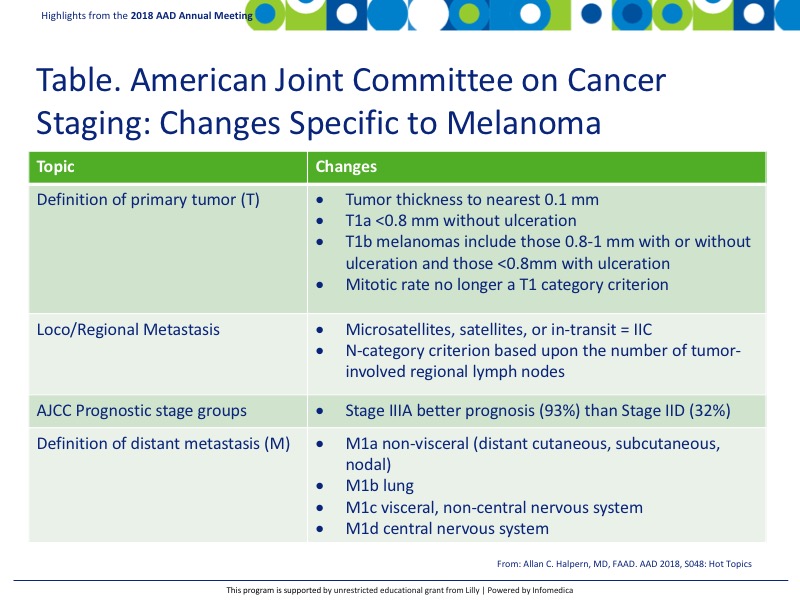
A new American Joint Committee on Cancer (AJCC) cancer staging manual is now available and is active as of January 2018. Changes specific to melanoma are reported in the following Table.
Dermoscopy is a non-invasive in vivo technique that allows visualization of subsurface structures of the skin that are not visible with the naked eye. Because dermascopes are relatively inexpensive, they can be readily integrated into routine primary care. However, the diagnostic accuracy of the dermascope is contingent on the skill of the user. Dermoscopy is routinely used among dermatologists in many countries. In contrast, only 48% of the 3,238 US dermatologists surveyed reported using dermoscopy in their practice in 2009.1 Dermatoscopy users in the US were more likely to be younger, involved in resident teaching, or have training in dermatoscopy.
Mobile dermatoscopes are now becoming more available. Full body dermatoscopes are useful for monitoring the progression of nevi as well as clearly identifying where on the body a specific nevus is located.
Artificial intelligence (AI) and computer technology is becoming more prevalent as there is a wiki and websites that have demonstrated high accuracy in the identification of malignant and benign lesions. On one such website, almost 130,000 clinical images were uploaded from more than 2000 diseases.2 In addition, the accuracy of the findings was on par with 21 tested dermatology experts thus revolutionizing the web approach for learning, identifying, and classifying normal and abnormal cutaneous lesions.
The International Skin Imaging Collaboration (ISIC) is a partnership with academia and industry to facilitate the clinical application of digital skin imaging with an initial focus on skin cancer, specifically melanoma. The initiative will help develop standards and allow the digital aspect of dermoscopy to bloom in US dermatology offices. Every year there are challenges to different countries that use the technology and compare it to expert dermatologists. In the 2016 challenge, only 3 dermatology experts were above the Area Under Curve (AUC) while the remaining were in line with AI.3 The 2017 challenge showed consistent performance between the dermatology experts and AI. These programs will shed light on lesions and propel patients to visit with their local dermatologist for treatment while being useful resources for both dermatologists and residents.
In melanomas, dysregulation of the Mitogen Activated Protein Kinase (MAPK) pathway occurs frequently due to activating mutations in the BRAF gene or other genetic or epigenetic modifications, leading to increased signaling activity promoting cell proliferation, invasion, metastasis, migration, survival and angiogenesis.
BRAF inhibitors have demonstrated effectiveness in mutant metastatic melanoma as more than 40% of melanomas have the same mutation in BRAF.4 However, with the addition of an MEK inhibitor, tumor cells were doubly subdued, while the downstream proliferation was minimized leading to successful outcomes.4
The use of nivolumab (PD-1 inhibitor) with ipilimumab (CTLA-4 inhibitor) has shown a considerable progression-free survival (PFS) in patients with metastatic melanoma.5 Data demonstrated durable responses for an extended period (15-18 months), which is considerable as traditional metastatic melanoma patients do not survive this long. However, it also came with a significant toxicity profile. Nivolumab was recently awarded adjuvant treatment status of melanoma. PD-1 class of agents has also demonstrated PFS with a safer toxicity profile than CTLA-4.5 The most prevalent toxicities include rash, pruritus, liver toxicity, diarrhea, colitis, and hypophysitis.
Key Messages
- The new AJCC has been released and is active as of January 2018. Main changes from the last version include primary tumor definition, metastasis definition and explanation, and staging.
- Dermoscopy is gaining popularity in the US and should be a regular tool used by dermatologists. Both portable and full body dermoscopy units are invaluable in identifying and monitoring normal/abnormal skin nevi/lesions.
- Treatment for metastatic melanoma includes the incorporation of inhibitors for BRAF and MEK as well as immunotherapies that limit the effectiveness of the immune system. However, with this limitation, toxicities may occur as a direct result of turning off the immune system and should be carefully considered when determining treatment options.
REFERENCES
Present disclosure: The presenter has reported that he has done work for Canfield Scientific, Inc. and Caliber ID.
Written by: Debbie Anderson, PhD
Reviewed by: Victor Desmond Mandel, MD
